November 4, 2014
 By Dennis ThompsonHealthDay Reporter
By Dennis ThompsonHealthDay Reporter
Latest Alzheimers News
FRIDAY, Oct. 31, 2014 (HealthDay News) — Malfunction of a key brain protein called tau is the likely culprit behind Alzheimer’s disease and other forms of dementia, a new study in mice concludes.
Neurons — highly specialized nerve cells in the brain — appear to die when tau malfunctions and fails to clear the cells of unwanted and toxic proteins, explained Charbel Moussa, head of the Laboratory for Dementia and Parkinsonism at Georgetown University School of Medicine, in Washington, D.C.
This means drugs that replace the function of tau in these brain cells are likely to slow the progression of Alzheimer’s, he said.
“A strategy like this will give us hope that we can delay or stabilize the disease progression,” Moussa said.
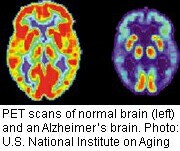
Tau has long been a prime suspect in the search for the cause of Alzheimer’s disease. The brains of Alzheimer’s patients wind up clogged with twisted protein threads made of tau, particularly in regions important to memory.
But researchers have been at a loss to explain why tau might cause Alzheimer’s, and whether the tangles of tau are more important than another hallmark of Alzheimer’s, plaques made of a protein called amyloid beta that fill the spaces between the brain’s nerve cells.
Moussa said his experiments with mice have shown that tau works to keep neurons naturally free of amyloid beta and other toxic proteins.
When tau malfunctions, the neurons begin to spit amyloid beta out into the space between the brain cells, where the protein sticks together and forms plaques, he said.
“When tau does not function, the cell cannot remove the garbage,” Moussa said. The result is cell death, he explained.
Tests on the brain cells of mice revealed that removing all tau impaired the neurons’ ability to clear out amyloid beta, according to findings published Oct. 31 in the journal Molecular Neurodegeneration. But if researchers reintroduced tau into brain cells, the neurons were better able to remove accumulated amyloid beta from the cells.
Moussa said his study suggests the remaining amyloid beta inside the neuron destroys the cells, not the plaques that build up outside. The mouse experiments also showed that fewer plaques accumulate outside the cell when tau is functioning.
Malfunctioning tau can occur as part of the aging process or due to genetic changes. As people grow older, some tau can malfunction while enough normal tau remains to help clear the garbage and keep neurons alive. “That explains the confusing clinical observations of older people who have plaque buildup, but no dementia,” Moussa explained in a Georgetown University news release.
In this study, Moussa also explored the possible use of a cancer drug called nilotinib to force neurons to keep themselves free of garbage, with the help of some remaining functional tau.
“This drug can work if there is a higher percentage of good to bad tau in the cell,” added Moussa, whose work was funded in part by a grant from Merck & Co., the pharmaceutical company.
Heather Snyder, director of medical and scientific operations for the Alzheimer’s Association, said Moussa’s findings are interesting but not conclusive.
“They’re saying that tau may have an earlier role than we currently know. That’s as far as I would go,” Snyder said. “We still don’t know how all the pieces come together.”
Snyder said new imaging technology that allows doctors to track tau buildup in a person’s brain over time may help solve this question in the future.
Also, experts say, results of animal experiments don’t necessarily apply to humans.
But Dr. Ronald Petersen, director of the Mayo Clinic Alzheimer’s Disease Research Center, said the new study adds to the growing evidence that “the role of tau is fundamental in the disease process.”
“Developing therapeutics for tau is a high priority,” Petersen said. “Not easy, not simple, but it could be very fruitful.”
 Copyright © 2014 HealthDay. All rights reserved.
Copyright © 2014 HealthDay. All rights reserved.
SOURCES: Charbel Moussa, Ph.D., assistant professor and head, Laboratory for Dementia and Parkinsonism, Georgetown University School of Medicine, Washington, D.C.; Heather Snyder, Ph.D., director, medical and scientific operations, Alzheimer’s Association; Ronald Petersen, M.D., Ph.D., director, Mayo Clinic Alzheimer’s Disease Research Center, Rochester, Minn.; Georgetown University, news release, Oct. 31, 2014; Oct. 31, 2014, Molecular Neurodegeneration
![]()